In a new publication from LVPEI, Drs. Amrita Mohanty, Srikant Kumar Sahu, and others describe the long-term management and outcomes of a unique type of immune stromal keratitis caused by microsporidia infection.
Doctors specializing in corneal infections often struggle with a treatment paradox: they must manage both the infectious agent and the body’s immune response to it. The cornea is a transparent layer of the eye that also functions as an ocular barrier to dust and pathogens. Any breach in the ocular barrier can cause infection by pathogens such as bacteria, viruses, fungi, or parasites, which triggers the host’s immune response and inflames the cornea—a condition known as keratitis. This inflammation is usually restricted to the outer layer, or epithelium, of the cornea and can also be self-limiting. Sometimes, the infection triggers an inflammation in the stroma, the fibrous middle layer of the cornea, leading to a blinding condition called immune stromal keratitis (ISK). This condition causes dense scarring and abnormal blood vessel formation in the cornea, resulting in severe vision loss. ISK can happen either due to direct infiltration of pathogens into the stroma or an immune response triggered by antigens—molecules that trigger immune responses—retained in the cornea even after the microbes fall below a threshold capable of causing an infection. The complex nature of ISK pathogenesis makes it poorly understood.
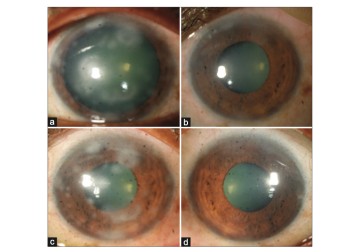
Microsporidia is a class of parasitic, spore-forming fungi known to infect the cornea—either the epithelium or the underlying stroma—triggering a vicious form of keratitis. However, recent evidence shows that it can do more than that. One study from LVPEI found that even a diffuse presence of microsporidia or other pathogens (say, an adenovirus) on the corneal surface can induce ISK, an event that is distinct from typical microsporidial infection of the cornea. Microsporidia-induced stromal inflammatory keratitis (MISIK) had a much quicker response to topical steroids, reducing inflammation in two weeks. The previous study described the clinical features, diagnosis, and management of MISIK in detail. However, the long-term outcomes of the condition and its treatment were unknown.
In a brief communication published in the Indian Journal of Ophthalmology, Drs. Amrita Mohanty, Srikant Kumar Sahu, and others from LVPEI describe the management and outcomes of MISIK after long-term follow-up. The retrospective study included the medical records of 20 patients diagnosed with MISIK who received at least 3 months of care, with a majority getting over 6 months of follow-up. Steroid eye drops and 0.03% tacrolimus ointment—an immunosuppressant—were prescribed to the patients to help reduce inflammation.
The patients had a follow-up duration that ranged from 100 days to 23 months. MISIK continued in 11 (55%) of the 20 patients for more than three months. Nine (82%) of those 11 patients had stopped using the prescribed medication too soon, after the acute inflammatory phase of ISK subsided. This led to recurrent inflammation in five (55%) of those nine patients—exactly six inflammatory episodes in roughly four months after discontinuing medication. A microbiological assessment confirmed the reappearance of microsporidia spores. The patients were advised to restart using steroid eye drops and topical tacrolimus. Restarting medication stopped the recurrent inflammation, with no new episodes observed over the next six months. This study, along with the previous paper, is among the first to report a new type of eye inflammation and underscores the importance of following through with medication as per the doctor’s advice.
‘Microsporidia ocular infections can manifest as epithelial and stromal infection and stromal inflammation, each having varied clinical manifestation and specific management,’ notes Dr. Amrita Mohanty, the first author of this paper and consultant ophthalmologist at LVPEI. ‘We present evidence for a treatment protocol that does not require any medication that directly tackles the infection; managing the inflammation alone works.’
Citation
Mohanty, A., Behera, H. S., Das, S., Fernandes, M., Parida, P., & Sahu, S. K. (2025). Management and outcome of microsporidia-induced stromal inflammatory keratitis - A long-term follow-up study. Indian Journal of Ophthalmology. Advance online publication. https://doi.org/10.4103/IJO.IJO_1141_24
Photo credit: Fig. 1, Mohanty et al.