Sohini Mandal and colleagues from LVPEI comment on the learning curve involved in performing Descemet Membrane Endothelial Keratoplasty during fellowship training.
The cornea is a transparent, multilayered outer segment of the eye that bends light inwards. Its innermost structure are two specific layers that help maintain corneal transparency: the Descemet’s membrane (DM) and an endothelial barrier. DM is the ‘basement’ membrane, which is around 10 microns thick (1/10th the thickness of a hair strand). The endothelial layer is a single sheet of barrier cells that lie on DM. When either of these layers are damaged, the cornea swells leading to vision loss. To restore clear vision, surgeons perform a minimally invasive procedure known as the Descemet Membrane Endothelial Keratoplasty (DMEK). They replace these damaged layers with the same layers from a healthy donor tissue. DMEK has revolutionized care by offering faster visual recovery, better anatomical restoration, and lower rejection rates compared to older methods.
However, DMEK is not an easy procedure to perform. It requires precision and finesse to handle these delicate sub-layers at the back of the cornea. And so, skill at performing DMEK comes with a steep learning curve. Learning DMEK techniques can be challenging for corneal fellows early in their surgical training. Postoperative complications like graft detachment, fibrin formation and pressure related issues can result from error. It is therefore necessary to understand what could lead to better training outcomes among surgeons learning to perform DMEK.
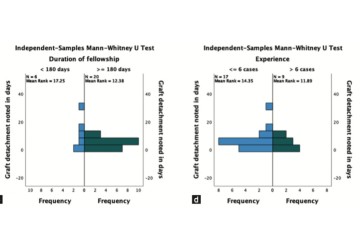
A retrospective commentary published in the Indian Journal of Ophthalmology by Sohini Mandal and colleagues from the L V Prasad Eye Institute analyzed 65 DMEK surgeries performed by 8 fellows during their fellowship training. The study divided the fellows as beginners (less than or equal to 6 DMEK surgeries) and experienced (over 6 surgeries). Of the 65 surgeries, 41 were performed by beginners and 24 by experienced fellows. They also grouped the surgeries by training duration: 17 surgeries were performed by fellows during their early training phase (
The study found that graft detachment occurred across all groups and was influenced by several factors, including case complexity and postoperative care. Fibrin formation—a sign of excessive handling—was seen only in surgeries performed by beginners. Although fellows in the late-training group showed good visual outcomes overall, the study revealed that the strongest predictor of better results was not time spent in training, but the actual number of DMEK surgeries performed. Fellows who had completed more than six surgeries consistently achieved better postoperative visual acuity than those with fewer cases, regardless of their fellowship duration.
‘Understanding how cornea fellows acquire DMEK skills is essential, because each step on the learning curve directly influences patient outcomes. Our study shows that structured exposure and hands-on experience—not just time in training—are the key drivers of surgical success,’ notes Dr Sohini Mandal, consultant ophthalmologist at LVPEI Mithu Tulsi Chanrai campus in Bhubaneshwar, and this study’s first author.
Citation
Mandal, Sohini; Deshmukh, Vishwajeet; Priyadarshini, Smruti Rekha; Das, Sujata; Sahu, Srikant Kumar. Navigating the learning curve in Descemet membrane endothelial keratoplasty – Insights from fellowship training. Indian Journal of Ophthalmology 73(10):p 1533-1536, October 2025. | DOI: 10.4103/IJO.IJO_1167_25
Photo credit: Fig. 1, duration of fellowship vs. experience, Mandal et al.