In a new study from LVPEI, Anshuman Verma, Mrinal Singh, Sunita Chaurasia and others map eye symptoms and its genetic causes in xeroderma pigmentosum (XP), reporting 12 novel XP-C variants and identifying XP-E variant for the first time in the Indian population.
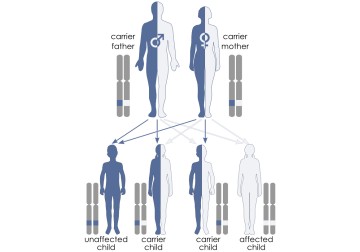
Young Ameer Hamza dreams of being a pilot but stepping into sunlight is dangerous for him. In the documentary, Father Will I See Again?, the teenager’s daily routine is shaped by him avoiding daylight – a cap, black glasses, full sleeves and jeans. Brown spots dot his skin, the marks of Xeroderma Pigmentosum (XP). A rare genetic condition with no cure, XP makes Ameer extremely sensitive to UV light. Even minimal sun exposure results in severe sunburns, freckle-like spots, and premature ageing of skin, with a high risk of cancer and neurological damage too. Caused by defects in a DNA repair pathway that fixes UV-induced damage, it has eight known genetic subtypes. XP’s incidence rate remains unknown in India. A major risk factor for XP is consanguinity (union between two biologically related individuals). The impact of XP on vision, while less prominent than skin damage, is equally harmful.
The eyes are constantly exposed to light. Like most healthy tissues, the eye too has an ability to repair itself from some degree of UV exposure. In people with XP, the skin or the eyes have an impaired ability to repair from UV exposure, accumulating damage over time. Early eye symptoms often go unnoticed, as people focus on the more visible skin changes that occur. By the time eye problems are recognized, the damage tends to be severe. Many children with XP develop cataracts, tumors on the eyelids, or vascular changes on the cornea. If not diagnosed early, it can lead to blindness or visual impairment--Ameer had developed corneal scarring too, in the movie. What genetic pathways drive XP in kids like Ameer?
In a new study published in Cornea, Anshuman Varma, Mrinal Singh and others from LVPEI examined 23 patients (15 men) with XP. Of the 23 patients, 16 were born to consanguineous parents. All patients had photophobia (sensitivity to light) and visual impairment along with facial and skin pigmentation. Common ocular findings included conjunctival abnormalities (98%), corneal involvement (80%), and eyelid changes (70%). Ocular surface dryness was reported in 17% of patients and over a third of patients (37%) had growth on the surface of the eyelids – signs of ocular surface neoplasia (OSN) that can precede cancer.
The researchers identified disease causing variants using whole exome sequencing (WES), a method used to determine the protein coding regions of the genome. The analysis revealed 15 XP-C variants of which 12 were novel. They also detected three XP-E variants, reported for the first time in the Indian population. This variant was associated with higher ocular risk as all three patients with the XP-E variant developed OSN. The authors stress on early diagnosis, genetic counselling especially among consanguineous partners, and increasing public awareness of genetic testing. Sun protection and regular eye checkups could slow the progression of this incurable disease. Ameer’s sight was restored through a corneal transplant, showing how access to specialized care can improve quality of life for people with XP.
'The significance of genetic testing in Xeroderma patients with ocular involvement lies in linking clinical eye findings to genetic subtypes, allowing early diagnosis and timely intervention,' says Sunita Chaurasia, consultant ophthalmologist at LVPEI and corresponding author of the paper.
Citation
Verma A, Singh M, Ramappa M, Ali H, Chaurasia S. Ocular Manifestations and Genetic Spectrum of Xeroderma Pigmentosum: Insights From an Indian Cohort in a Global Context. Cornea. 2026 Feb 1;45(2):223-231. doi: 10.1097/ICO.0000000000004013. Epub 2025 Oct 8. PMID: 41236424.
Photo credit: Autosomal recessive inheritance, Thomas Shafee, CC BY 4.0