In a collaborative study between LVPEI and The University of Alabama, USA, Srijita Kundu, Sanhita Roy and others report on the expression of key molecular markers associated with tissue damage in mucormycosis cases.
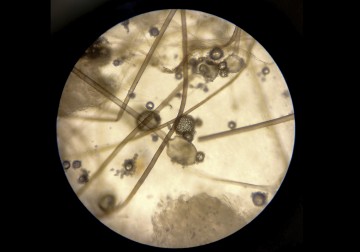
The COVID-19 pandemic caused by the SARS-CoV-2 virus unleashed a complex set of secondary ‘syndemics’ in 2021. India also reported a surge in mucormycosis - a rare, fast-spreading, life-threatening fungal infection. This rise was driven by factors like uncontrolled diabetes and widespread use of corticosteroid as part of COVID-19 treatment. Popularly referred to as the ‘black fungus disease’, it primarily affects people with weakened immune systems. The most common and severe form, rhino-orbital cerebral mucormycosis (ROCM), begins in the sinuses and can spread to the eyes and brain within days. It has a high mortality rate, reaching upto 80% once it invades the brain, and the road to recovery is hard even for survivors. In 2021, more than 3,000 deaths were attributed to COVID-19–associated mucormycosis (CAM). An aggressive infection, mucormycosis causes extensive tissue damage leaving little time to intervene once it takes hold.
One of the processes underlying this damage is oxidative stress. When tissues are infected, cells respond by producing chemically reactive molecules called reactive oxygen species (ROS). Under normal conditions, antioxidants keep ROS in check and maintain cellular balance. In people with diabetes, this balance is disrupted. High blood sugar creates conditions favorable for fungal growth while weakening the immune system’s ability to control infection. In severe infections like mucormycosis, this balance is further impaired. Excessive ROS in tissues damage proteins, lipids and DNA pushing the cells into oxidative stress. This could trigger programmed cell death (PCD) - a set of controlled, self-destruct pathways that act as ‘cellular executioners’. Despite the aggressive nature of the disease, the cellular and molecular events that cause it to spiral with such speed and severity remain poorly understood.
In a new study published in Medical Mycology, Srijita Kundu, Sanhita Roy and colleagues from LVPEI analyzed eye and orbital tissues (removed surgically) from 14 patients with RCOM, including 10 with CAM, and compared them with uninfected control tissues. It was noted that 92.8% of patients had diabetes. Viral proteins from SARS-CoV-2 were detected in 71% of CAM patients, even in those who had recovered from COVID earlier. The researchers analyzed markers of oxidative stress and various PCD pathways using immunofluorescence staining.
The tissues showed clear signs of oxidative stress along with activation of multiple cell-death pathways detected through the increased expression of various proteins associated with these mechanisms. These changes were seen irrespective of the patient’s COVID status. The findings suggest that while COVID 19 may increase susceptibility to the infection through factors like steroid use, the processes that cause tissue damage is intrinsic to the infection itself. The study sheds light on how the body responds to mucormycosis, thereby providing a basis for developing targeted therapies beyond antifungals that could regulate tissue damage and improve outcomes for high-risk patients.
‘Mucormycosis is a deadly fungal infection with high death rate, therefore it is extremely essential to study the disease pattern in host cells to identify cellular targets for future treatments,' remarked Dr. Sanhita Roy, Head of Ocular Pharmacology Research at LVPEI and corresponding author of the paper.
Citation
Kundu S, Riegler AN, Chelappan R, Mishra DK, Dave TV, Leal SM Jr, Roy S. Immunohistochemical insights into oxidative stress and programmed cell death in primary and COVID-associated rhino-orbital-cerebral mucormycosis patient tissues. Med Mycol. 2025 Nov 4;63(11):myaf104. doi: 10.1093/mmy/myaf104. PMID: 41206545.
Photo credit: Mucor, Artemyev Danila, CC By 4.0