In a new clinical trial at LVPEI, Drs. Rashmi Deshmukh, Pravin K. Vaddavalli, and others describe the efficacy, safety, and outcomes of Xenia porcine corneal lenticules in eyes with advanced keratoconus after one year of implantation.
Keratoconus is a progressive eye disorder marked by the gradual thinning of the cornea, the transparent front part of the eye, which bulges into a cone. The progressive distortion of the cornea’s shape causes blurry vision and, without treatment, can end in severe vision impairment. When diagnosed early, the progression of keratoconus can be stopped. Collagen crosslinking (CXL), a minimally invasive procedure in which the interaction between UV light and riboflavin is used to ‘crosslink’ and strengthen collagen fibers in the cornea, is a common and effective intervention for stalling keratoconus. Once halted, corrective contact lenses or glasses can be used to improve visual acuity. Collagen crosslinking can be combined with intracorneal ring segments or photorefractive keratectomy to regularize the cornea and improve vision. However, these treatments can only be used if the stroma, the cornea’s collagen-rich middle layer, has sufficient thickness. Treatment options in advanced keratoconus, where the cornea becomes too thin, are limited and may end up requiring invasive surgery such as corneal transplantation (keratoplasty).
Corneal lenticular implantation, or stromal keratophakia, has emerged as an alternative for treating advanced keratoconus. In this procedure, a thin, disk-shaped lenticule of corneal tissue is harvested from a donor and inserted into a small pocket—created using a femtosecond laser—within the patient’s corneal stroma. The implant adds thickness and helps regularise the patient’s cornea, thereby improving vision. Recently, xenogeneic corneal implants—lenticules from other species—have come into play, reducing the need for scarce human corneas. Xenia® implants are decellularized xenogeneic lenticules derived from pig corneas due to their similarity to human corneas. The lenticules are crosslinked multiple times during manufacturing to improve strength, while decellularization minimizes the risk of implant rejection. Xenia® promises to be an effective alternative to keratoplasty in advanced keratoconus. But is it truly effective?
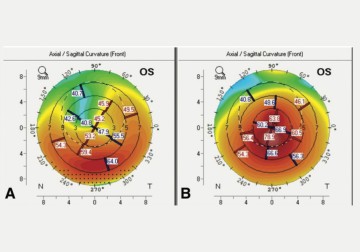
In a new, open-label clinical trial published in the Journal of Refractive Surgery, Drs. Rashmi Deshmukh, Pravin K. Vaddavalli, and others from LVPEI report the efficacy, safety, and outcomes of Xenia® lenticules in advanced keratoconus one year after implantation. The lenticules were implanted in nine eyes of nine patients with advanced keratoconus not suitable for CXL. Corneal topography was used to measure the cornea’s curvature and thickness, to assess the outcomes after one year.
Distance visual acuity (DVA), or visual clarity at a distance, improved after lenticule implantation. On average, uncorrected DVA improved from 1.43 logMAR to 0.78 logMAR, which demonstrates a significant visual improvement. With corrective spectacles, DVA further improved to 0.45 logMAR. Topography scans showed that the patients’ corneas underwent significant flattening after a year from the lenticule implantation. None of the patients had an implant rejection. However, the stroma in two eyes showed signs of ‘melting,’ needing an explant and requiring further intervention. Overall, Xenia® lenticules show promising results and the potential to be an effective, minimally invasive treatment for advanced keratoconus, but the implant still needs further refining.
'Porcine collagen implants are good, novel alternatives to human donor corneal lenticules in the management of advanced keratoconus, however, the procedure needs refining and long term follow ups need to be looked at,' notes Dr Rashmi Deshmukh, the first author, and consultant ophthalmologist at LVPEI.
Citation
Deshmukh, R., Mohan, R. M., Madonadi Kuniyil, V., & Vaddavalli, P. K. (2025). Porcine Collagen Implants in Advanced Keratoconus: Outcomes at 1 Year. Journal of Refractive Surgery (Thorofare, N.J.: 1995), 41(3), e272–e279. https://doi.org/10.3928/1081597X-20250207-02
Photo credit: Fig. 1, Deshmukh et al.