In a new study from LVPEI, Drs. Sunita Chaurasia, Jessica Daza and others have described the strategies and outcomes of a modified style of compression suture in acute corneal hydrops.
The cornea is made of three transparent layers: the outer layers of cells (epithelium), the middle—and the thickest—layer of collagen (stroma), and a single layer of cells (endothelium) which grows on a thin Descemet's membrane along the inner surface of the cornea. Conditions like keratoconus or pellucid marginal corneal degeneration (PMCD) are marked by weakened biomechanics and structural instability of the cornea. In some severe cases, this instability can result in a break of the inner membrane, with fluids from the interior leaking into the cornea. The accumulated fluid buildup turns the cornea hazy leading to vision loss—corneal hydrops. Hydrops can clear naturally, but it can take weeks or even months. If hydrops persists, it can lead to complications like abnormal proliferation of blood vessels into the cornea, or lazy eye (amblyopia) in children. So, a quick resolution of hydrops through medical intervention is the wiser option.
A common approach to treating acute hydrops is injecting gas (e.g., sulfur hexafluoride) into the anterior chamber of the eye. The gas acts as a tamponade, a band-aid that keeps the Descemet's membrane attached to the corneal stroma, sealing any leaks. But the injected gas can cause complications such as elevated intraocular pressure, risk of early cataracts, abnormal pupil dilation (Urretts-Zavalia syndrome), and degeneration of the iris. The patient also needs to hold their face in awkward positions, which can be uncomfortable. For all that effort, the gas tamponade too would take weeks to patch the breaks in membrane. Full-thickness compression sutures are another option with a lower risk of complications. These sutures bind the torn edges of the Descemet's membrane, reducing the size of the tear. However, the deeper layers are difficult to access, and the risk of surgery-induced complications creeps in. What if there is a better way to do these sutures?
In a new prospective interventional study published in the journal Cornea, Drs. Sunita Chaurasia, Jessica Daza and others describe the techniques and outcomes of a modified style of compression sutures in corneal hydrops. The study examines partial-thickness sutures, about 50-60% from the corneal surface. It included 28 patients (29 eyes) with acute hydrops who underwent the experimental procedure. Twenty-three (82%) patients had hydrops due to keratoconus, while the rest had PMCD. All patients had poor vision (only moving hands) before surgery.
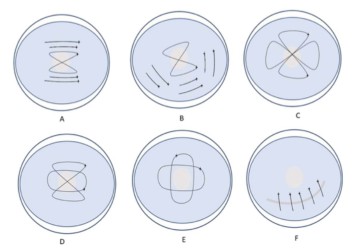
The team evaluated partial-thickness suturing in six different patterns based on the shape, position, and size of membrane breach. After surgery, fluid-induced swelling (corneal edema) reduced by 76% in one day, by 92% in a week, and by 99% in three weeks. The sutures were removed, on average, 48 days after surgery. None of the patients developed any suture-related complications. The patients were rehabilitated with corrective eyewear. Spectacles and contact lenses improved the visual acuity of 20 eyes from blindness to moderate (15 eyes) or mild vision impairment (5 eyes). The study establishes the safety and efficacy of partial thickness sutures and opens new avenues for hydrops management.
‘Partial-thickness compression suturing is a simplified technique for managing large hydrops,’ concludes Dr. Sunita Chaurasia, Medical Director of the Ramayamma International Eye Bank at LVPEI and the corresponding author of this paper. ‘In patients with PMCD, this intervention can also lead to improved vision.’
Citation
Daza, J., Ramappa, M., Murthy, S., & Chaurasia, S. (2024). Strategies and Application of Compression Sutures with a Modified Technique for Rapid Resolution of Large (Grade III) Hydrops: A Prospective Interventional Study. Cornea. Advance online publication. https://doi.org/10.1097/ICO.0000000000003496