Dr Tarjani Dave and her colleagues from L V Prasad Eye Institute discuss a retrospective analysis of patients who underwent evisceration and primary implant surgery using Electronic Medical Record data. The paper reports on the outcomes of 1800 patients over seven years—the largest such series to date.
The end-stage management of a severely damaged eye is its evisceration, where the contents of the eye are removed while preserving the scleral shell and extraocular muscle. Unless dealing with ocular tumors, evisceration has come to replace enucleation, where the entire globe is removed. Evisceration has benefits for both the surgeon and the patient: it saves time, is cost-effective, and the patient’s prosthesis moves in response to muscle impulse leading to better cosmetic outcomes. Improved surgical techniques with scleral flaps and optic nerve disinsertion have led to better outcomes and custom ocular prosthesis for the patients.
Several evisceration techniques have been refined over the decades, and these refinements have addressed complications like arrested prosthetic motility, infections, sunken or displaced implants. However, there is little empirical data describing the complications due to evisceration and implant outcomes across the world. After evisceration, surgeons have the choice to use porous or non-porous implants on which to mount the ocular prosthesis. While many surgeons use cost-effective non-porous implants, data on the outcomes of such implants is also scarce, leading to some questions on its risks. A previous study from LVPEI noted that there was no increased risk of implant migration when a non-porous implant is used along with ‘two-petal’ sclerotomy. However, a large tranche of empirical data will be key to answering these questions definitively.
A recent investigation by Dr Tarjani Dave and others in The International Journal on Orbital Disorders, Oculoplastic and Lacrimal Surgery presents the largest series of patients who have undergone evisceration with implants to date. The paper analyses the electronic medical records (EMR) of 1800 patients who underwent evisceration surgery with primary implants at LVPEI from 2013 to 2019. Most patients were male (64%) and 16% were children. Nearly 97% (1737 cases) of the patients received non-porous polymethyl methacrylate (PMMA) implants, while the remaining 3% received porous polyethylene implants. Additionally, two-petal sclerotomy was performed in 88% of cases.
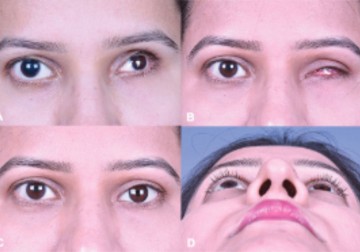
The study found trauma to the eye as the most common cause requiring evisceration surgery. Implant complications such as exposure and extrusion were seen in only 3% of cases. The study found that about 2% of the eyes with PMMA implants had displacement—but did not require intervention, as it did not hinder prosthesis. The paper reports that evisceration with an implant (mean diameter: 20mm) leads to fewer complications and good cosmetic outcomes in 93% of the patients covered. Just as important, the study records a median patient satisfaction score of 8 out of 10 with the prosthesis.
'This study has a key, public health message: trauma is the most common risk factor for evisceration and many patients in our study tended to be younger. Simple interventions like wearing protective glasses while working on farms and industries would go a long way in preserving eyes and vision,' says Dr Tarjani Dave, lead author and consultant ophthalmologist at LVPEI.
Citation
Tarjani Vivek Dave, Anthony Vipin Das, Sameer Mohapatra, Oshin Bansal & Anasua Ganguly (2022) Outcomes and complications of evisceration with primary implant: an electronic medical record driven analytics of 1800 cases, Orbit, 41:6, 717-725, DOI: 10.1080/01676830.2021.1998915
Photo credit: Assessing the aesthetic outcomes of evisceration and implant; Dave et al.