A review paper by Drs Swati Singh and Sayan Basu from L V Prasad Eye Institute, India and Dr Gerd Geerling, University Hospital Dusseldorf, Germany explores salivary gland transplantation as an alternative strategy for the treatment of Dry Eye Disease (DED). The paper provides a detailed overview of the anatomy of the lacrimal and salivary glands, salivary gland transplantation techniques, and the treatment outcomes and complications of these techniques for patients with DED.
Lacrimal gland secretions are necessary to maintain a healthy ocular surface. Insufficient tears lead to ocular diseases like Dry Eye Disease (DED), with tear film instability and chronic inflammation. Various ocular conditions can lead to permanently damaged lacrimal glands in patients, completely drying up the ocular surface—a condition called severe aqueous tear deficiency (ATD). ATD patients will need to frequently use lubricants but may still report poor quality of life and discomfort. ATD will also damage the cornea and impair vision over time. Saving their vision will require keratoplasty or even stem cell transplantation—but they may not have adequate lubrication to ensure a successful intervention.
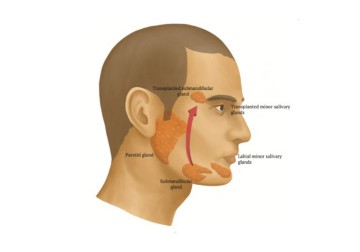
Salivary glands around the mouth are like lacrimal glands; some of them produce mucoserous secretions that are similar to tears. This is especially true of the submandibular glands that reside right under the jaw. However, they are not a perfect match; the proteins that make up the two secretions and their osmolarity differ substantially. Starting from the 1950s, attempts have been made to graft one (or a portion) of the salivary glands to produce ‘salivary tears’ in patients with damaged lacrimal glands. These complex, microvascular procedures are a marvel of human surgical ingenuity. There are now several types of procedures with varying degrees of outcomes.
A review paper by Dr Swati Singh and her colleagues in The Ocular Surface provides a comprehensive overview of salivary gland transplantation techniques for restoring tear volume in patients with severe Dry Eye Disease (DED). The paper compares the anatomy of salivary and lacrimal glands, various transplantation techniques, and the outcomes & complications of each of them. It discusses specific surgical techniques (in animal models and humans) for salivary gland transplantation—namely the submandibular gland transplantation (SMGT) and minor salivary gland transplantation (MSGT)--and evaluates the viability of the two procedures for treatment of patients with severe DED. It systematically presents the steps involved in each of these procedures, including variations, and their outcomes with good-quality illustrations, and histological and slit lamp images.
The paper carefully sifts through the available records for these techniques, noting the advantages and outcomes of both. It notes for example that SMGT is a complex procedure needing an ophthalmologist and an oral maxillofacial surgeon, while MSGT requires an ophthalmologist alone. SMGT leads to 85-100% graft viability and good Schirmer values (a test to determine the moisture of the eye’s surface), however the salivary tears produced are hyposmolar: their protein content is far lower than regular tears. In contrast, MSGT achieves 95% graft viability. There is also some improvement in visual acuity. The transplanted tissue seems to maintain long-term functional architecture. However, the overall lubrication volume produced after this procedure is lower. The paper notes the need to better evaluate outcomes and to help choose the best approach for patients with absolute ATD, where all other solutions are inadequate.
'The restoration of tear volume in patients with severe lacrimal gland damage still remains a challenge,’ says Dr Swati Singh, the lead author and Assistant Ophthalmologist, Centre for Ocular Regeneration, LVPEI. ‘Salivary gland transplantation has paved the way for exploring the dream of transplanting the lacrimal gland instead, in the future.’
Citation
Singh S, Basu S, Geerling G. Salivary gland transplantation for dry eye disease: Indications, techniques, and outcomes. Ocul Surf. 2022 Aug 7;26:53-62. doi: 10.1016/j.jtos.2022.07.013. Epub ahead of print. PMID: 35948165.
Photo credit: Fig. 1. Distribution of salivary glands and their transplanted locations, by Singh et al.