In a collaborative study between LVPEI and the Royal Victorian Eye and Ear Hospital, Melbourne, Australia, Rashmi Deshmukh, Pravin Krishna Vaddavalli and others evaluate risk factors for treatment failure in patients with keratoconus.
Keratoconus, a rare sight-threatening condition, develops when the cornea loses its structural strength. The exact cause of keratoconus is still not fully understood, but it often begins in adolescence and is seen in men more than women. Collagen fibres in the cornea, the transparent outermost layer of the eye, help it maintain strength and shape. In patients with keratoconus, the bonds between these collagen fibers begin to weaken, and the cornea thins and bulges outward into a cone. The steepest longitudinal meridian of the cornea increases measurably as the condition progresses, distorting vision. Strengthening the collagen bonds, therefore, stops and reduces this progressive outward bulge, and is central to keratoconus treatment.
Collagen cross-linking (CXL) is the only known surgical technique which induces chemical bonds that strengthen the weakened collagen fibres of the cornea. The procedure uses ultraviolet-A light to stimulate a photosensitizer like riboflavin (Vitamin B2) added to the cornea. The activated riboflavin molecules induce new chemical bonds between the collagen fibers, stiffening the tissue. This action halts the bulging cornea and prevents the progression of keratoconus in most cases. While CXL has become a standard of care for keratoconus, some post-procedure patients may have a recurrence after a few years.
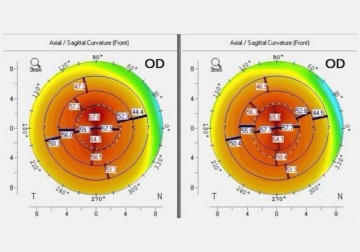
A recent study published in Cornea by a team from LVPEI led by Dr. Rashmi Deshmukh examined patients whose keratoconus worsened despite undergoing a CXL procedure. It included 31 eyes from 30 patients whose keratoconus progressed and compared them to 40 eyes from 32 patients who remained stable for more than five years. Most of the patients had a central bulge, while a few patients in both groups had an eccentric bulge. A key measure was a parameter called maximum keratometry (Kmax), which measures the steepest curve (longitude) of the cornea. The mean Kmax in the control group was about 62.94 dioptres (along with other parameters).
The study found that eyes with steeper corneas at the start of the study were more likely to advance despite treatment. This suggests that the severity of keratoconus before CXL influences the procedure’s outcomes. Of the 31 eyes, 20 with a mean Kmax of 66.53 dioptres underwent a repeat CXL and remained stable after a follow-up of three years. The other 11 eyes were too advanced to undergo CXL again and required a corneal transplant. Four eyes with a mean Kmax of 73.9 dioptres underwent a partial thickness corneal transplant while 7 eyes with a mean Kmax of 87.1 dioptres required a full-thickness corneal transplant. Other factors, like age or allergic eye disease, did not seem to impact the likelihood of primary CXL failure. Nearly 80% of the patients who required a secondary procedure had a central bulge.
‘The idea was to understand the outcomes when primary crosslinking fails. There was nothing definitive in our population. The factors associated, and outcomes for progressive keratoconus despite undergoing crosslinking were unknown’, notes Dr. Rashmi Deshmukh, consultant ophthalmologist and scientist at LVPEI and first author of the study. ‘This study helps understand the risk factors for progression despite primary collagen crosslinking and provides insights for improving long-term vision outcomes for patients with keratoconus.’
Citation:
Deshmukh R, Heroor A, Singh S, Vaddavalli PK, Vajpayee RB. Evaluation of Clinical Profile and Management Modalities in Eyes With Progressive Keratoconus After Primary Collagen Cross-Linking. Cornea. 2025 Jul 1. doi: 10.1097/ICO.0000000000003926. Epub ahead of print. PMID: 40591368.
Photo credit: Fig. 1, Deshmukh et al.