In a new study from LVPEI, Drs. Amrita Mohanty, Bhupesh Bagga, and others describe the clinical features, management, and outcomes of infectious crystalline keratopathy, a rare ocular infection that can happen after a cornea transplant.
Infections are the most common risk associated with eye surgeries. This is especially true for a corneal transplant, or keratoplasty, in which a damaged cornea is replaced with a healthy one from a donor. An infection, following this procedure, can lead to rejection of the grafted tissue, disruption of wound healing, and an overall poor outcome. Infectious crystalline keratopathy (ICK) is an infection resulting from bacteria colonizing a cornea after keratoplasty, that can result in graft failure. ICK causes unique greyish-white, needle-like branches to spread across the cornea, turning it opaque.
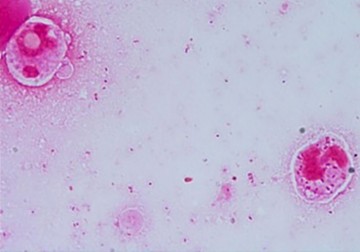
ICK is usually caused by Streptococcus viridans, though other types of gram-positive and gram-negative bacteria, and less commonly fungi, can also trigger it. Despite the infection, patients with ICK present with minimal ocular inflammation and are treated with antibiotics. Corticosteroids, often prescribed after a keratoplasty to manage inflammation, are also discontinued because localized immune suppression by steroids can increase the risk of microbial infection. However, early aggressive treatment with antibiotics according to antimicrobial sensitivity and stopping topical steroids is often adequate, avoiding an immediate therapeutic transplant. Developing a more effective treatment for ICK is critical, but before that, it is necessary to better understand the complexities of the condition.
In a new study published in the journal International Ophthalmology, Drs. Amrita Mohanty, Bhupesh Bagga, and others from LVPEI describe the clinical features, management, and outcomes of ICK. The retrospective study included 24 cases of ICK (62.5% of which were men), recorded over an 11-year period. Most (18, or 75%) of the patients had undergone keratoplasty before the infection and had large corneal grafts (10.1+/-1.5 mm). On average, the patients with ICK came to LVPEI 9.7 months after their corneal graft. The research team also compared the data from the ICK patients to 24 cases of other corneal infections after keratoplasty that are characterized by graft infiltrates (GI)—opaque aggregations of inflammatory cells inside the cornea, a sign of corneal infection.
Compared to GIs, most patients with ICK (75%) showed less symptoms of infection and sought medical attention, on an average, 9 days later. Patients with ICK also had smaller corneal infiltrate sizes (less than 4mm), and over 70% of them were positioned at the cornea’s center. Only two patients (9%) had pus accumulation in the anterior chamber of the eye (hypopyon) while another two had a perforation in their cornea. Patients with ICK were also frequently using topical steroids (over 3 times a day). Twenty-two out of 24 cases of ICK were microbial culture positive. Among those, 63.6% of ICK were due to gram-positive bacteria, 13.6% were due to gram-negative bacteria, and 9% were due to mixed bacterial infection. Interestingly, 13.6% of cases were fungal infections. Most patients (79.2%) recovered with medicine, while five patients required a new corneal graft. The study concludes that ICK is more likely to manifest after keratoplasty among patients with large corneal grafts and with frequent use of steroid eye drops.
'ICK is a unique cause of infection—mostly bacterial—among cornea transplant patients, and we are getting to know its characteristics in finer detail,' says Dr. Amrita Mohanty, consulting ophthalmologist at LVPEI and the first author of this paper. 'Apart from a compromised immune response because of long-term steroid use, we noted that the size of the graft is a key risk factor. The good news is that it responds to medication.'
Citation
Mohanty, A., Joseph, J., Mishra, D. K., Pasha, A. A., & Bagga, B. (2024). Infectious crystalline keratopathy-clinical-microbiological profile and outcome of management. International Ophthalmology, 44(1), 343. https://doi.org/10.1007/s10792-024-03267-7
Photo credit: Gram-positive cocci and gram-negative coco-bacilli, Mohanty et al.