In a new study from LVPEI, Drs. Sohini Mandal, Sujata Das, and others report that inflammation is not associated with the degree of infection in microsporidia stromal keratitis.
The cornea, a transparent, multi-layered tissue in the front of the eye, can be a target of various infectious pathogens—bacteria, viruses, fungi, and even parasites. Microsporidia, a group of spore-forming parasites, seems to prefer the gastrointestinal tract and the eye, among other organs in the human body. Microsporidial infection of the cornea, or microsporidia keratitis, usually happens from exposure to contaminated water and is typically a self-resolving condition if the infection is limited to the outer layer (epithelium) of the cornea. However, if the pathogen manages to penetrate the corneal stroma, the fibrous middle layer of the cornea, things can escalate into a vision-impairing inflammation called microsporidia stromal keratitis (MSK).
MSK is an insidious condition, developing slowly but with lasting effects. Its symptoms are diffuse, varying based on the causative genus, often leading to misdiagnosis and delayed treatment. The damage to the eye could be because of the persistent infection, the prolonged inflammation from the body’s immune response, or a combination of both. Even after a correct diagnosis, treatment options are limited. The only reliable treatment is a cornea transplant, or penetrating keratoplasty, an invasive surgery that is dependent on the availability of donor corneas. What drives MSK progression despite antimicrobial treatment? Is it lingering pathogens or persistent inflammation?
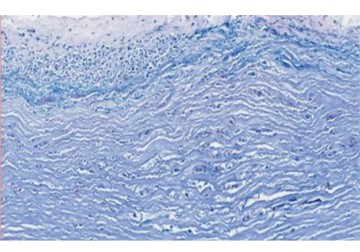
In a new study published in the journal Investigative Ophthalmology & Visual Science, Drs. Sohini Mandal, Sujata Das, and others from LVPEI address that question by unraveling the histopathological features of MSK from infected corneal buttons—disc-shaped pieces of cornea—obtained during keratoplasty. The retrospective, consecutive case series included 22 corneal buttons from 22 patients diagnosed with MSK over an 8-year period. Along with histopathological analysis—morphology, degree and distribution of inflammatory cells, etc.—the researchers also looked at the microbiology of the infected corneas.
The researchers observed several morphological changes in the infected cornea, such as ulcers in the epithelium, thinning of the stromal layer, and even necrosis (large-scale cell death) of the stroma. Corneal inflammation is marked by the aggregation of inflammatory cells. These cells were detected in 21 corneal buttons, and in most cases, inflammation was present in all layers of the cornea. Microbiological smear assessment showed that only 59% (13 cases) of the corneal buttons had microsporidia spores. However, microscopic examination of the buttons revealed the spores, either diffusely present or localized in one part of the stroma—emphasizing the unreliability of microbial smear tests at detecting microsporidial infections. In the end, the researchers found no association between inflammation and the distribution of microsporidia in the corneas. Inflammation did not correlate with the severity of infection, either. However, the symptoms of MSK lasted significantly longer in cases with moderately severe infections. The lack of proportional inflammatory response to the presence of microsporidial spores underscores the complex nature of MSK. It is possible that the slow and sneaky nature of microsporidia helps it evade the immune system for a long time before inflammation finally kicks in, resulting in a disassociation between the two factors. Only further research can explain the underlying cause behind the lack of correlation.
‘This study from LVPEI, Bhubaneswar, represents one of the most comprehensive histopathological evaluations of corneal tissues affected by microsporidia stromal keratitis to date,’ says Dr. Sohini Mandal, Consultant Ophthalmologist at LVPEI and the lead author of the paper. ‘By correlating clinical findings with histopathological evidence, it deepens our understanding of the pathobiology of this rare infection, refines diagnostic certainty, and informs surgical decision-making. As a center of excellence in corneal care, LVPEI is proud to contribute such seminal work to the global literature—work that enhances scientific insight.’
Citation
Mandal, S., Sucharita, S., Deshmukh, V., Priyadarshini, S. R., Sahu, S. K., & Das, S. (2025). Histopathological Evaluation of Corneal Tissues in Microsporidia Stromal Keratitis. Investigative Ophthalmology & Visual Science, 66(4), 9. https://doi.org/10.1167/iovs.66.4.9
Photo credit: Fig. 2 F, Mandal et al.