In a new retrospective study, Drs. Rashmi S. Deshmukh, Pravin K. Vaddavalli, and Anthony V. Das presented the changing trends in presentation, diagnosis, and treatment of keratoconus within the LVPEI network over the last three decades.
Keratoconus is an eye condition usually found in young people. The transparent, dome-shaped front of the eye, the cornea, progressively thins and bulges out into a conical shape. This corneal distortion manifests as myopia and astigmatism, causing blurred vision. Keratoconus can disrupt the most productive period in a young person’s life. It is important then to identify the condition early and plan its management and treatment to prevent sight loss. For many decades, patients sought medical help late into their 30s, and there was a limited set of diagnostic and therapeutic tools.
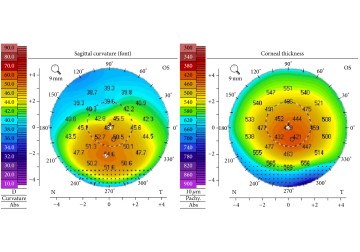
Over time, diagnostic technologies have exploded: from the keratoscope (a simple reflection-based imaging tool) to corneal topography which generates a 2D image of the cornea, to 3D corneal tomography. Treatment options have also improved. For decades, a full-thickness corneal transplant was the main treatment. Today, corrective contact lenses can manage almost half of all keratoconus cases. Minimally invasive surgeries like collagen crosslinking (CXL), which uses UV rays to crosslink and strengthen the corneal collagen fibers, are also being used to arrest keratoconus progression. In more serious cases, deep anterior lamellar keratoplasty (DALK) can be used to replace only the affected layers of the cornea, making it less invasive and more viable than a full corneal transplant. With such a range of diagnostic and therapeutic options, there is a sea-change in the practice patterns among Indian ophthalmologists who treat keratoconus.
A new retrospective study published in the journal Cornea by Drs. Rashmi S. Deshmukh, Pravin K. Vaddavalli, and Anthony V. Das reports on the changing trends in presentation, diagnosis, and treatment of keratoconus within LVPEI over the last 33 years (1987-2020). The study included 20,576 patients with keratoconus, who came to LVPEI in the 33-year period. Most patients were men (61.25%). Among the changing trends, the average age of diagnosis for keratoconus reduced from 29.3 years (between 1987 and 1991) to 22.2 years (between 2012 and 2020). More patients were also being diagnosed with keratoconus over time: while only 173 patients were diagnosed with keratoconus between 1987 and 1991, over 7400 patients were diagnosed between 2017 and 2020.
The use of contact lenses in keratoconus management has also increased over time, especially the scleral and hybrid lenses. Between 2002 and 2006, contact lenses were used to treat only 4.34% of keratoconus patients. That increased to 11.23% between 2016 and 2020—a 2.5-fold rise in 14 years. CXL became the preferred surgical intervention: between 2007 and 2011, CXL made up only one-fifth (22.28%) of all surgeries performed to treat keratoconus. That number increased to more than half (53.61%) from 2012 to 2016, and then to almost three-quarters (72.53%) between 2017 and 2020. In fact, CXL made up over 85% of surgical interventions for keratoconus at LVPEI over an eight-year period (2012-2020). Even in cases which required corneal transplantation, more patients underwent the less-invasive DALK (1.72%) than full-thickness corneal transplant (1.04%), between 2012 and 2020.
‘Our understanding of keratoconus has improved over the last few decades which has led to significant developments in the diagnostic trends and treatment strategies,’ concludes Dr. Rashmi S. Deshmukh, Consultant Ophthalmologist at LVPEI and the first author of this paper. ‘Our study highlights the evolution of the presentation and management of keratoconus over the past three decades.’
Citation
Deshmukh, R. S., Das, A. V., & Vaddavalli, P. K. (2024). Evolving Trends in the Diagnosis and Management of Keratoconus Over 3 Decades. Cornea. Advance online publication. https://doi.org/10.1097/ICO.0000000000003635
Photo credit: Elise A. Slim et al., CC BY 4.0, via Wikimedia Commons.